3 Dangerous Hormone Myths that Harm Women
Doctors still believe these myths, and women suffer because they aren't set straight
*IV Ketamine, NR, and NAD+ have been used clinically off-label for decades. They are not FDA approved for the treatment of any psychiatric or pain condition. All medical treatments carry risks and benefits that you must discuss with a doctor at Clarus Health to learn if these therapies are right for you.

These three hormone myths are still taught – and they’re quietly harming millions of women every day
I treat women's health conditions that most of my patients have been gaslit over for years. Here are the three prevailing myths that prevent my patients from getting the care they deserve.
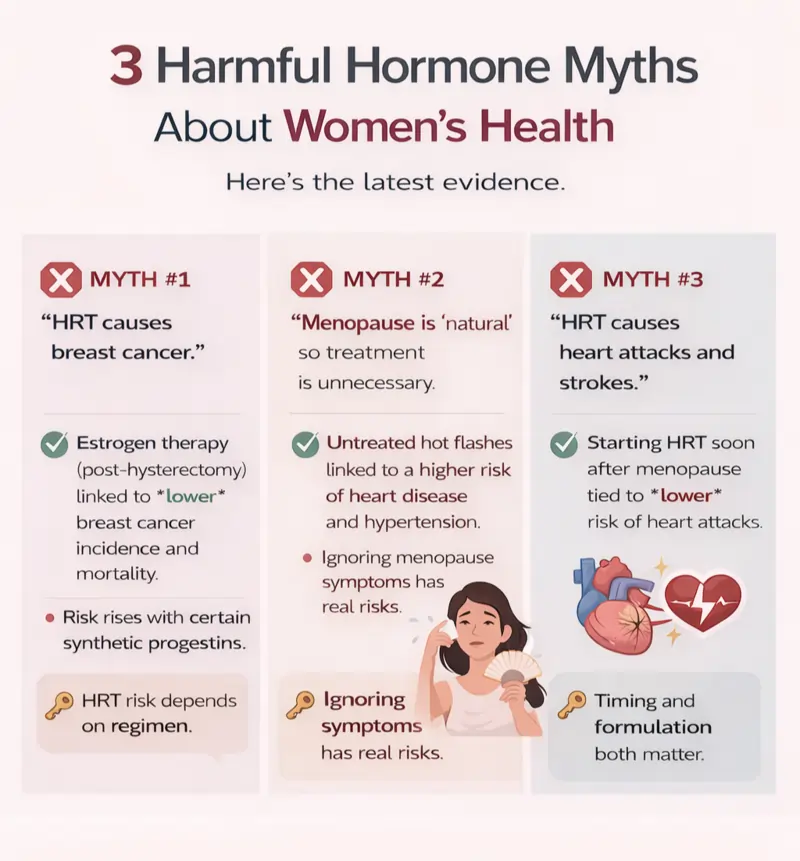
Myth #1: “Hormone replacement therapy causes breast cancer”
This is the most common fear I hear, and it’s the one that causes the most unnecessary suffering. The problem is simple: “HRT” is not one drug. Risk depends on the specific regimen, and the data look very different for estrogen-only therapy versus estrogen plus certain synthetic progestins.
What the data actually shows (estrogen-only)
In long-term follow-up from the Women’s Health Initiative (WHI) randomized trials, women with prior hysterectomy who received estrogen-only therapy had lower breast cancer incidence and lower breast cancer mortality compared with placebo.
A 2024 meta-analysis of randomized trials also concluded that estrogen-alone therapy is associated with a reduction in breast cancer incidence in the randomized evidence base.
Where HRT risk differences become real: the “progesterone” piece
Most women with an intact uterus need endometrial protection when using systemic estrogen. That’s why clinicians add a “progesterone-like” hormone to HRT, and this is where a major risk can arise.
Large observational cohorts suggest that synthetic progestins are more consistently associated with increased breast cancer risk than micronized (bioidentical) progesterone, which appears to show a lower risk signal in several datasets. These are not perfect studies, but they are clinically meaningful, and ignoring them is not “being cautious,” it’s being imprecise.
Modern HRT and Breast Cancer Risk: the practical takeaway
Saying “HRT causes breast cancer” without specifying the regimen is simply inaccurate. A responsible discussion includes:
- which estrogen (and dose),
- which route (oral vs transdermal),
- which progestogen (micronized progesterone vs a specific progestin),
- your individualized baseline risk.
Myth #2: “Hormones naturally decline, so treating menopause is unnecessary (or dangerous)”
“Natural” does not mean “benign.” Bone density loss is natural. Muscle loss is natural. Rising insulin resistance can be natural. We still treat osteoporosis, sarcopenia, diabetes, and hypertension because ignoring them causes pain and disease.
Menopause symptoms deserve the same respect. If symptoms are significant - think sleep disruption, mood instability, brain fog, worsening quality of life - dismissal is not medicine.
Ignoring hormone health may cause real cardiovascular harm, because hot flashes can be damaging to your heart.
Hot flashes aren’t just annoying - they can damage your heart
Hot flashes and night sweats, called "vasomotor symptoms," are associated with measurable cardiometabolic signals in multiple studies. For example:
- Hot flashes are associated with higher estimated insulin resistance
- Vasomotor symptoms are also associated with greater aortic calcification and poorer endothelial function - increasing cardiovascular risk
- Autonomic dysfunction from hot flashes appears to increase the risk of high blood pressure
Not treating natural hormone decline has risks: the practical takeaway
If menopause is impairing your sleep, mood, cognition, relationships, or work, that is not “optional” suffering. It deserves a real risk–benefit discussion - not dismissal.
Myth #3: “Hormone therapy causes heart attacks and strokes”
This myth survives because there is some truth, but this is far from a blanket statement.
Timing and formulation matter. Starting therapy earlier after menopause tends to have a different risk profile than starting much later, when heart disease is more established. This concept is often called the “timing hypothesis.”
Hormone Replacement Therapy May Actually Reduce Heart Attack Risk
In a Danish randomized trial involving recently postmenopausal women, women receiving hormone replacement therapy had fewer heart attacks without any apparent increase in risk of cancer, blood clots, or strokes.
What to do with the stroke and blood clot concern
Hormone replacement therapy carries real risks, particularly for certain women and certain formulations (especially oral estrogen at higher doses or initiation later after menopause, and in those with elevated clot risk). That’s why competent care is individualized. The goal is not “hormones for everyone.” The goal is the right regimen, for the right person, at the right time, with appropriate monitoring.
Heart Attacks and Strokes with HRT: the practical takeaway
When timed properly, hormone replacement therapy is unlikely to increase heart attack or stroke risk - it may even lower the risk based on some studies.
Five questions to ask your doctor for safer hormone replacement therapy
- Am I within the “earlier initiation” window (age and time since menopause)?
- What is my baseline risk for clots/stroke and breast cancer (family history, prior events, smoking, etc.)?
- If I have a uterus, which progestogen are you recommending, and why that one?
- Would transdermal estrogen be safer for my risk profile than oral?
- What is the follow-up plan (symptom targets, labs if indicated, dose adjustments, and clear stop rules)?
Is Bioidentical Hormone Replacement Therapy Right For You?
Discussing hormones with your doctor isn't optional, it can be lifesaving. Used thoughtfully, HRT can improve symptoms and function. Used carelessly, it can cause harm. Withheld because of myths, it can also cause harm.
If you’ve been denied a nuanced conversation, that is not a “you” problem. It’s a standard-of-care problem.
Learn more about your hormone health and longevity goals by speaking with a doctor at Clarus Health today.




