Ketamine for Treatment-Resistant Depression... and Why Hormone Optimization Improves Results
Ketamine Therapy can rapidly improve depression while naturally balancing hormone health for lasting improvement
*IV Ketamine, NR, and NAD+ have been used clinically off-label for decades. They are not FDA approved for the treatment of any psychiatric or pain condition. All medical treatments carry risks and benefits that you must discuss with a doctor at Clarus Health to learn if these therapies are right for you.

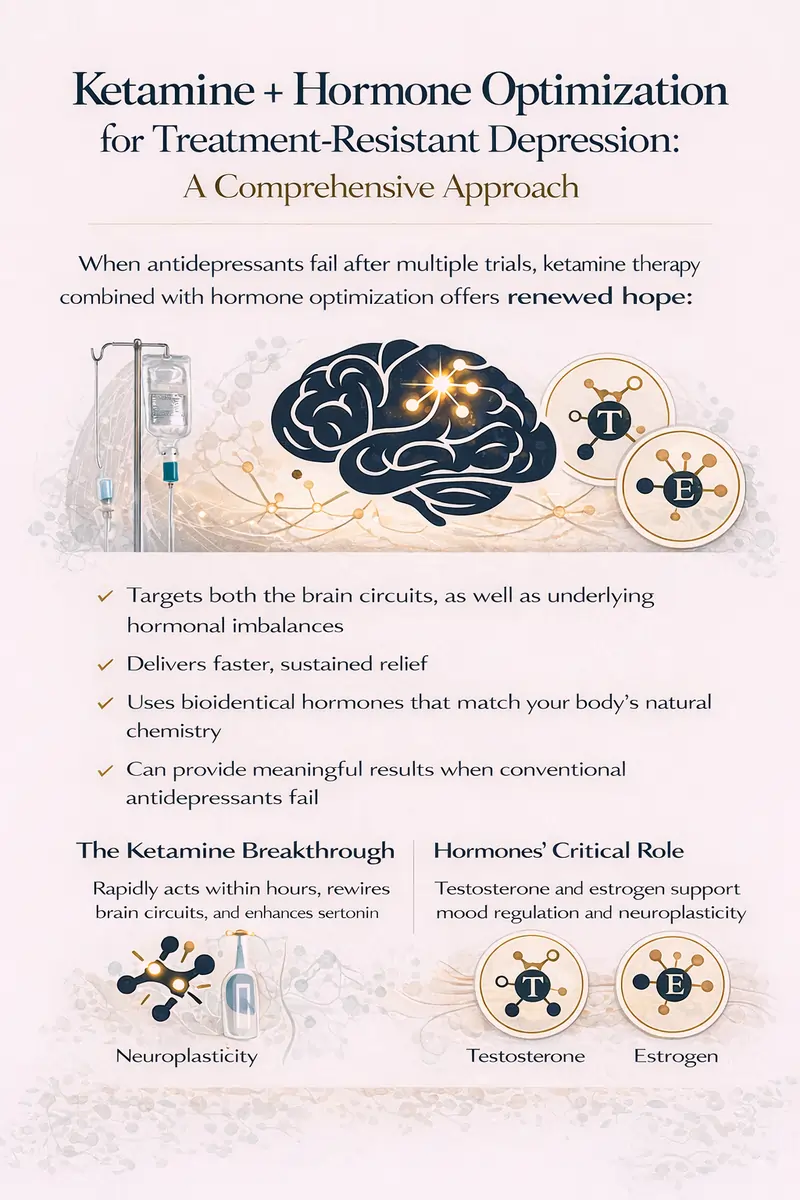
Ketamine + Hormone Optimization for Treatment-Resistant Depression
When antidepressant medications fail to work after multiple attempts, the diagnosis becomes treatment-resistant depression (TRD). Nearly 3 million Americans face this challenging condition, where traditional treatments offer little relief. But emerging research points to a powerful combination: ketamine therapy paired with hormone optimization.
Hormones Can Affect Treatment-Resistant Depression
Treatment-resistant depression affects approximately 12-20% of people with major depressive disorder. It's defined as depression that doesn't respond adequately to at least two different antidepressant medications. The emotional and physical toll is immense - patients experience persistent sadness, fatigue, difficulty concentrating, and an inability to experience pleasure that can last months or years.
Clarus Health always tells patients they probably don't have a "Prozac deficiency" but there may be a hormone deficiency causing or worsening symptoms. Ketamine and hormone balancing can have a powerful synergy in these patients.
Dr. Kaveh tells his patients he's never seen a patient with a Prozac deficiency, but he has treated many hormone deficiencies!
The Ketamine Breakthrough for Depression
Ketamine represents a paradigm shift in depression treatment. Unlike traditional antidepressants that take 6-8 weeks to show effects, ketamine works within hours. Landmark research demonstrated significant improvement in depressive symptoms within just 2 hours of infusion, with 64% experiencing meaningful relief within 24 hours.
The mechanism is fundamentally different from conventional antidepressants. While most medications target serotonin or norepinephrine, ketamine works through the glutamate system (it blocks NMDA receptors). This triggers rapid formation of new neural connections in the prefrontal cortex, essentially rewiring circuits disrupted by chronic stress and depression.
Unlike traditional antidepressants, ketamine potently rewires neuron connections. This is called neuroplasticity and occurs within 12-24 hours and correlates directly with sustained mood improvement lasting days to weeks.
The Hormone-Ketamine Connection for Treatment-Resistant Depression
What makes hormone optimization a crucial companion to ketamine? Research from the National Institutes of Health reveals that sex hormones - particularly testosterone and estrogen - play essential roles in mood regulation and brain function.
Testosterone and Depression
Studies show that men with treatment-resistant depression often have suboptimal testosterone levels. Testosterone replacement may improve depression symptoms, particularly in men with dysthymic disorder, HIV, or already-low testosterone levels. Testosterone modulates serotonin receptor density in the brain and influences multiple neurotransmitter systems involved in mood regulation.
For women, testosterone is equally important despite being produced in smaller quantities. The most abundant biologically active hormone throughout the female lifespan, testosterone deficiency can manifest as irritability, anxiety, depression, fatigue, and poor concentration - symptoms that overlap significantly with major depression.
Estrogen's Role in Depression and Mental Health
Estrogen has profound effects on brain chemistry and emotional processing. Estrogen can modulate serotonin function, with serotonin responsivity decreasing after menopause and restoring following estradiol treatment. Periods of low estrogen - such as perimenopause and menopause - represent windows of heightened risk for depressive episodes.
The relationship between estrogen and depression follows a complex pattern. Women experience higher rates of depression than men, with hormonal fluctuations during reproductive transitions (pregnancy, postpartum, menopause) particularly associated with worsening depressive symptoms.
The Critical Difference: Bioidentical vs. Synthetic Hormones and Depression Risk
Not all hormone therapy is created equal, and this distinction is crucial for mental health outcomes. The type of hormones used - bioidentical versus synthetic - can make a profound difference in how patients respond, particularly regarding mood and psychiatric symptoms.
Synthetic Hormones and Mental Health Risks
Synthetic hormones, particularly those used in birth control, have been consistently linked to increased rates of depression and anxiety, especially in adolescents.
The mental health impact extends beyond depression. Progestogen-only contraception may create a greater propensity for depressive disorders in vulnerable women, with users reporting higher rates of anxiety, mood swings, and irritability. Recent proteomic analysis has revealed that synthetic sex hormones used in oral contraception induce changes in neural pathways related to inflammation, oxidative stress, and cell death - biological processes known to intersect with mechanisms implicated in depression.
These synthetic hormones have chemical structures that differ from the hormones naturally produced by your body. These structural differences lead to distinct and sometimes opposite physiological effects compared to bioidentical hormones.
Bioidentical Hormones: A Different Story for Depression
Bioidentical hormones - including estradiol, progesterone, and testosterone - have molecular structures identical to the hormones your body produces naturally.
Patients report greater satisfaction and favorable effects on depression and anxiety scores with bioidentical hormones, often with fewer side effects than synthetic hormones.
Your brain has evolved to respond to specific molecular structures - estradiol, progesterone, testosterone - and these are the signals it recognizes and responds to optimally!
Why Combine Ketamine and Bioidentical Hormone Therapy for Depression?
The ketamine and hormone synergy makes biological sense: ketamine rapidly restores neural connectivity and optimizing hormones supports nervous system health:
- Enhanced neurotransmitter function - Both testosterone and estrogen influence serotonin, dopamine, and other mood-regulating chemicals without the inflammatory effects of synthetic alternatives
- Supports neuroplasticity - Bioidentical hormones promote the formation and survival of new neural connections that ketamine initiates
- Addresses root causes - While ketamine provides rapid symptom relief, bioidentical hormone optimization corrects underlying biochemical imbalances without introducing synthetic compounds that may worsen mood
- Sustains improvements - Balanced bioidentical hormones help maintain the neural changes ketamine creates without the psychiatric side effects associated with synthetic hormones
Is Personalized Depression Treatment Right for You?
Combining IV ketamine therapy with bioidentical hormone optimization addresses both immediate symptoms (through ketamine's rapid action) and the underlying hormonal dysregulation that may perpetuate depressive symptoms - typically with fewer side effects.
Speak with a doctor at Clarus Health today to learn more about transforming your mental health for rapid and lasting changes.




