5 Dangerous Risks of Low Progesterone
The dangers of progesterone deficiency are real, but most doctors don't discuss this with their patients
*IV Ketamine, NR, and NAD+ have been used clinically off-label for decades. They are not FDA approved for the treatment of any psychiatric or pain condition. All medical treatments carry risks and benefits that you must discuss with a doctor at Clarus Health to learn if these therapies are right for you.

Progesterone is routinely treated as a “fertility hormone” or a minor add-on to estrogen. That view is outdated. Progesterone is a neurosteroid, an immune modulator, and a hormone with clinically meaningful effects on bone, blood vessels, brain, and the uterus.
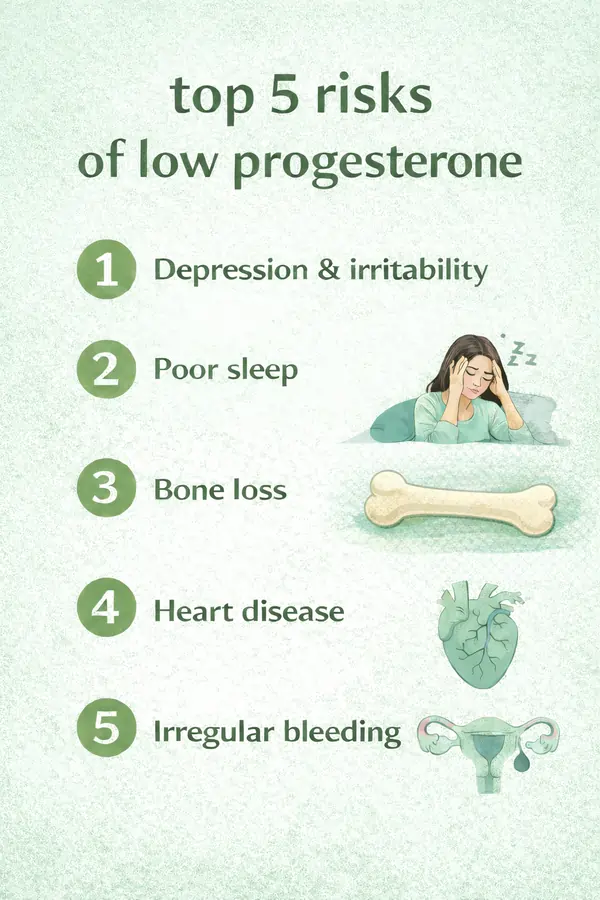
Below are five high-impact risks of low progesterone that are commonly missed - in both perimenopause and menopause.
What is progesterone?
Progesterone is one of the key reproductive hormones derived from cholesterol (a helpful pathway diagram is here). It is produced primarily by the ovaries, with contribution from the adrenal glands, and during pregnancy by the placenta. The nervous system also produces progesterone, which helps explain why progesterone can strongly influence sleep, anxiety, mood, and cognition.
Clinically, progesterone problems are not just about “low levels.” Some women develop progesterone resistance, where signaling at the receptor level is impaired - often in inflammatory states.
The 5 dangerous risks of low progesterone
1) Low progesterone may worsen depression, anxiety, irritability, and mood instability
Progesterone and its metabolites interact with brain systems involved in stress response and emotional regulation. During the menopause transition, women can be more vulnerable to depressive symptoms when hormone levels change. That being said, not all women are affected in the menopausal transition.
This is also where confusion arises between bioidentical progesterone and synthetic progestins. They are not interchangeable in brain effects. Large population data link hormonal contraception - a form of synthetic hormones - to increased depression risk in some groups.
2) Insomnia and sleep fragmentation
Sleep is one of the highest-yield clinical clues. Low progesterone commonly shows up as difficulty falling asleep, frequent awakenings, or non-restorative sleep, especially in perimenopause and menopause.
A systematic review/meta-analysis found micronized progesterone improves multiple sleep outcomes (particularly in postmenopausal women).
However, biology is not uniform. Some women experience paradoxical negative mood effects related to neurosteroid/GABA-A modulation.
3) Bone loss, osteoporosis, and fracture risk
Estrogen gets most of the attention, but progesterone matters in bone biology. Progesterone supports bone formation (osteoblast differentiation) and appears to work synergistically with estrogen.
If a patient’s bone density is declining, a serious evaluation asks not only “Is estrogen low?” but whether the overall sex-steroid environment, including progesterone signaling, is supporting bone remodeling.
4) Cardiovascular risk and vascular dysfunction
The vascular endothelium is central to atherosclerosis and cardiovascular disease, and progesterone appears to influence endothelial function and vascular regulation. Cardiovascular risk is multifactorial, but the clinical pattern is consistent: as sex-steroid signaling declines through menopause, cardiometabolic risk accelerates.
Progesterone is not a substitute for blood pressure, lipid, glucose, and lifestyle management, but ignoring hormone physiology can leave a key driver unaddressed in some patients.
5) Abnormal bleeding and endometrial hyperplasia risk
Progesterone counterbalances estrogen’s proliferative effects on the uterine lining. When cycles become anovulatory (common in perimenopause), progesterone can be functionally low relative to estrogen exposure, increasing risk of irregular bleeding and endometrial hyperplasia over time.
Irregular bleeding should not be normalized or ignored. It warrants evaluation, and progesterone physiology is often central to the explanation.
Why progesterone gets disrupted in modern life
Low progesterone (or progesterone resistance) is often downstream of broader stressors on the body:
Inflammation, metabolic dysfunction, and progesterone resistance are observed in women with endometriosis, PCOS, and other conditions.. Early-life and developmental conditions have also been linked to adult progesterone patterns.
Progesterone replacement can help, but route and formulation matter
The clinically important distinction is natural (bioidentical) progesterone versus synthetic progestins. Ovarian hormone dynamics correlate with mood symptoms in perimenopause, while synthetic hormonal contraception is associated with depression risk in some populations.
When menopausal hormone therapy is selected thoughtfully, evidence supports benefit for depressive symptom prevention during the menopause transition.
If oral progesterone causes unwanted neuropsychiatric effects in a subset of patients, alternate routes (including vaginal) may be considered in discussion with your doctor.
Is progesterone replacement right for you?
If someone has persistent insomnia, anxiety/depression symptoms, fatigue, brain fog, irregular bleeding, or bone loss, especially when symptoms cluster around perimenopause/menopause, progesterone signaling deserves evaluation. The goal is not chasing a single number; it’s assessing patterns, timing, inflammation, receptor signaling, and whether the formulation and route match the patient’s physiology. Speak with a doctor at Clarus Health today to learn if bioidentical hormone replacement therapy is right for you.




