Is Ketamine an Opioid? Understanding Ketamine and Addiction Risk
Is Ketamine an opioid with addiction risks? Both treat pain, but there are major differences in addiction potential...
*IV Ketamine, NR, and NAD+ have been used clinically off-label for decades. They are not FDA approved for the treatment of any psychiatric or pain condition. All medical treatments carry risks and benefits that you must discuss with a doctor at Clarus Health to learn if these therapies are right for you.

Patients regularly ask me "is ketamine an opioid?" when they are exploring ketamine therapy for depression, anxiety, PTSD, or chronic pain. While both medications can provide pain relief, ketamine is not an opioid - but it's important for you to understand the difference, especially in addiction potential of opioids compared to ketamine.
Over the last 30 years, ketamine therapy has become increasingly recognized as a powerful modality to heal severe mental health conditions and chronic pain. In this time, ketamine therapy has exploded in popularity, with celebrities like Chrissy Teigen, Lamar Odom, and Theo Von sharing their healing experiences. However, the tragic death of actor Matthew Perry has raised important questions about ketamine's safety and addiction potential.
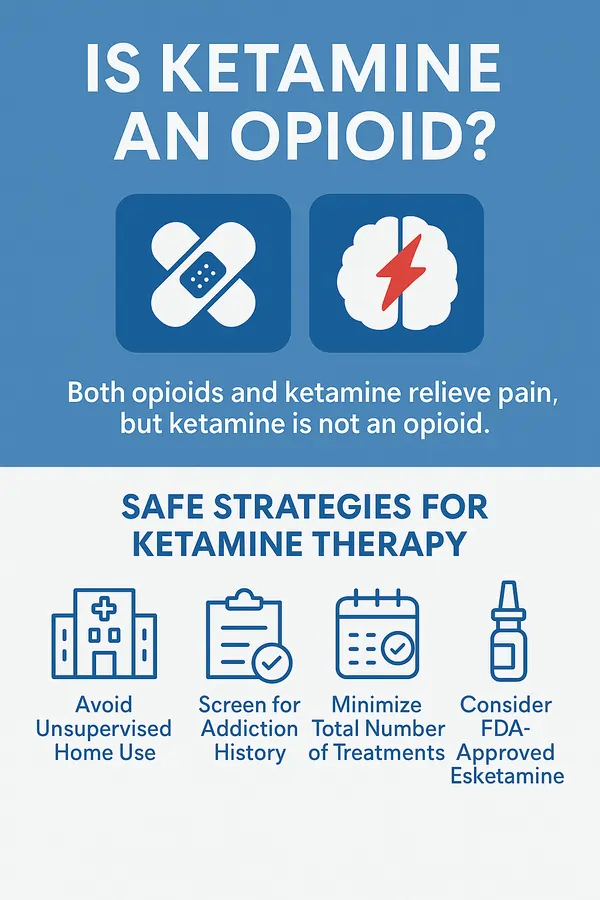
Is Ketamine an Opioid?
Ketamine is a 60-year-old, FDA-approved anesthetic medication that also provides pain relief. Unlike opioids, which bind to opioid receptors in the brain, ketamine functions as an NMDA receptor antagonist, affecting glutamate levels in the brain through a completely different mechanism.
Opioids like morphine, fentanyl, and oxycodone work by attaching to opioid receptors to block pain signals and trigger dopamine release. Ketamine works on NMDA receptors and glutamate pathways—a fundamentally different system in the brain.
The difference between ketamine and opioids is important because the risks are different. While more than 75% of drug overdoses in the USA involve opioids, ketamine-related overdose deaths remain under 1% according to CDC data.
Is Ketamine Addictive like Opioids? Understanding the Real Risks
Ketamine addiction is more nuanced than with opioid addiction. Research shows that risk of misuse and addiction appears very low in supervised clinical settings. However, the addiction landscape is changing as ketamine becomes more widely available.
Importantly, the risk of addiction for any medication is very different when used medically under supervision versus recreationally.
How Ketamine Addiction Differs from Opioid Addiction
Ketamine addiction affects the brain differently than opioid addiction because ketamine does not induce the same synaptic plasticity typically observed with addictive drugs, despite triggering dopamine release. It also doesn't cause traditional physical withdrawal symptoms like tremors, vomiting, or diarrhea seen with opioids.
Instead, ketamine withdrawal is primarily psychological. Some have described it as being "stuck in your head" with more mental distress than physical symptoms. So while ketamine can cause addiction changes to the brain, the risk appears lower than opioids.
Heavy recreational ketamine users consume more than 90 times higher doses than therapeutic use, which dramatically increases addiction risk and side effects. When doctors supervise ketamine therapy with much lower doses, addiction pathways appear less likely to activate.
IV Ketamine and FDA-approved esketamine are also used in office settings with direct doctor supervision - not at home. This supervised setting is another important difference in addiction risk between opioids and ketamine use.
Rising Trends in Ketamine Use
Despite the safety of ketamine, recent data reveals concerning trends. A 2025 study analyzing U.S. adults found that recreational ketamine use increased 81% from 2015 to 2019, and another 40% from 2021 to 2022. A study of recreational use in a nightclub in New York City also showed increased use of ketamine from 2017 to 20204.
Long-Term Side Effects of Ketamine vs Opioids: What You Need to Know
The two main long-term side effects of ketamine therapy are addiction and bladder injury (cystitis). The first report of bladder injury in medical use of ketamine occurred in a woman using ketamine lozenges and capsules for a year.
While we don't yet fully understand the mechanism, bladder inflammation appears to increase with more frequent ketamine use—another reason why minimizing total treatments is crucial. Fortunately, most cases appear reversible when ketamine use stops, though some can become permanent.
Strategies for Safe Ketamine Therapy for Depression, Anxiety, PTSD, and Chronic Pain
According to consensus guidelines published in JAMA Psychiatry, several strategies can greatly minimize risks:
1. Avoid Unsupervised Home Use
Medical experts strongly advise against at-home self-administration of ketamine. Supervised administration in a clinical setting remains the gold standard for safety.
2. Screen for Addiction History
Your doctor should carefully evaluate any history of substance use disorders. Interestingly, ketamine therapy can actually be helpful in patients with addiction, but close monitoring is essential to avoid trading one problem for another. This is still an area of active research.
3. Minimize Total Number of Treatments
Work with your doctor to maximize the benefit of each session, rather than scheduling frequent "booster" infusions. The goal should be getting the most therapeutic value from the fewest treatments possible.
4. Consider FDA-Approved Esketamine (Spravato)
For treatment-resistant depression, esketamine nasal spray is FDA-approved and covered by most major insurances. Clinical trials show significant effectiveness, and it may have even lower addiction risk compared to racemic ketamine, though this isn't yet definitively established.
The Ketamine-Opioid Connection: Emerging Research
While ketamine isn't an opioid, its antidepressant effects do include opioid receptors. Giving naltrexone (an opioid receptor blocker) can decrease the antidepressant effect of ketamine.
Paradoxically, research from 2025 shows ketamine may actually help treat opioid use disorder, reducing cravings and helping patients overcome fentanyl addiction. Ultra-low-dose ketamine has even been used to ease opioid withdrawal symptoms, offering new hope for addiction treatment.
The Bottom Line: Is Ketamine Safer than Opioids?
Ketamine is not an opioid, and when used responsibly under direct medical supervision, the risk of addiction appears very low. The medication shows tremendous promise for treatment-resistant depression, PTSD, anxiety, and chronic pain - conditions where traditional treatments often fall short and carry their own risks.
However, the explosion of online ketamine platforms raises legitimate concerns. Just as we witnessed with the opioid epidemic, predatory business practices can overshadow a medication's legitimate benefits. The key is finding qualified, ethical providers who:
- Provide in-person supervision during treatments
- Screen thoroughly for contraindications and addiction risk
- Focus on minimizing total treatments needed
- Discuss FDA-approved alternatives like Spravato
- Are transparent about risks, not just benefits
Speak with a doctor at Clarus Health today to learn if you are a candidate for IV ketamine therapy or Spravato to help healing from depression, anxiety, PTSD, or chronic pain.




