How Ketamine Affects Your Hormones (PMS and PMDD, too)
Ketamine can influence PMS and PMDD through estrogen, cortisol, and other hormones - what does that mean for your treatment?
*IV Ketamine, NR, and NAD+ have been used clinically off-label for decades. They are not FDA approved for the treatment of any psychiatric or pain condition. All medical treatments carry risks and benefits that you must discuss with a doctor at Clarus Health to learn if these therapies are right for you.

Ketamine therapy is best known for its rapid effects on depression, anxiety, and PTSD. But many patients - especially women - notice something else during treatment: changes in energy, sleep, mood, or symptoms tied to their menstrual cycle.
That’s not your imagination. Ketamine has real, measurable effects on hormones, particularly cortisol and estrogen-related brain signaling, which helps explain why ketamine therapy can feel different depending on where you are in your cycle -and why it may be especially relevant for PMS and PMDD.
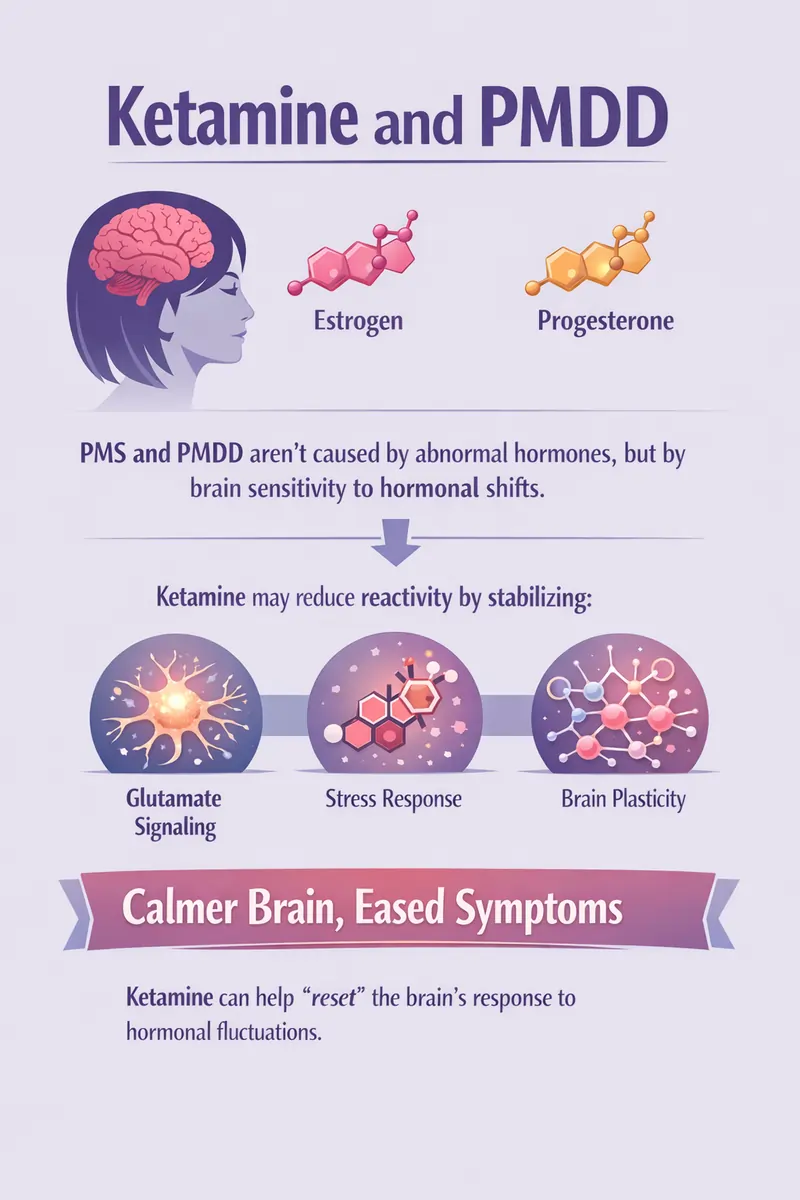
Ketamine, Estrogen, and the PMS–PMDD Connection
Estrogen doesn’t just affect the reproductive system - it strongly influences mood, glutamate signaling, and neuroplasticity.
Ketamine and its metabolites bind directly to estrogen receptor alpha (ERα) in the brain. When estrogen and ketamine are present together, they amplify AMPA receptor signaling, a pathway central to ketamine’s antidepressant effects.
Ketamine's interaction with estrogen receptor has important implications for women:
- Low estrogen states (late luteal phase, menopausal, etc.) may change how ketamine feels
- Estrogen fluctuations, not absolute levels, are a core driver of PMS and PMDD symptoms
- Ketamine may interact differently with the brain depending on cycle timing
Why Women with PMDD may Respond Well to Ketamine
PMDD is not “severe PMS” - it’s an abnormal brain response to hormone fluctuations (especially estrogen and progesterone). Because ketamine acts on the same glutamate and plasticity pathways influenced by estrogen, it may help “reset” maladaptive signaling during hormonally vulnerable windows.
Ketamine and Cortisol: Why You May Feel “Activated” After Ketamine Therapy
Ketamine reliably causes a temporary rise in cortisol, the body’s main stress hormone. But this doesn't occur in patients under anesthesia, only if they perceive the dissociative effects of ketamine.
The increase in cortisol is stronger in patients receiving ketamine for surgery, but this also occurs in patients receiving ketamine for depression. For many patients, this can feel like:
- Increased alertness or clarity
- Temporary restlessness
- Difficulty sleeping the night of treatment
This cortisol rise is brief, not chronic, with patients returning to baseline within hours. This partially explains why some patients, especially with PMS and PMDD, may feel better immediately, while others feel temporarily “wired” before improving.
Ketamine Also Affects Prolactin and Testosterone
Ketamine can also cause temporary increases in prolactin and luteinizing hormone.
The increase in luteinizing hormone is interesting because it may help support testosterone levels. In patients receiving ketamine for surgery, testosterone levels decrease with surgery, and post-operative ketamine may help support this important anabolic hormone.
These effects of ketamine on prolactin and leutinizing hormone are short-lived and not associated with long-term hormone disruption.
Ketamine Therapy and Hormones: Timing and Context Matter
Interestingly, ketamine only raises stress hormones when the experience is consciously perceived. When ketamine is given under general anesthesia, cortisol does not rise.
This suggests that the subjective experience - not just the medication - matters. This is why mindset, environment, and integration are especially important for hormonally sensitive patients.
Practical Takeaways for Patients Considering Ketamine Therapy
If you have PMS, PMDD, or hormone-related mood symptoms, here’s what matters:
- Ketamine therapy does interact with hormones, especially cortisol and estrogen signaling
- Effects are temporary and adaptive, not damaging
- Cycle timing may influence how treatment feels
- Hormone status should be part of personalized ketamine care - not glossed over
You should always discuss your hormone health with your doctor when considering ketamine therapy, both IV ketamine and Spravato.
Start Healing Today with Ketamine Therapy
Ketamine therapy doesn’t just affect mood: it engages the brain’s hormone-sensitive pathways. For patients with PMS or PMDD, this interaction may be part of why ketamine can feel powerful, nuanced, and sometimes different from other treatments.
Speak with a doctor at Clarus Health today to learn if IV ketamine is right for your depression or hormonal fluctuations.




